The National Disability Insurance Scheme (NDIS) plays a key role in supporting people with disability across Australia, helping them live safer, healthier and more independent lives. Yet many participants continue to face elevated health risks due to barriers in access, communication challenges, and co-existing health conditions. Health emergencies such as avoidable hospital admissions often occur when early signs are missed or when support is not consistently monitored.
This is where regular check-ins become essential. Whether delivered through scheduled visits, health assessments or ongoing wellbeing monitoring, they serve as a vital safety layer to prevent health emergencies among NDIS participants.
In this article, you will learn why regular check-ins matter, how they work within the NDIS framework, Kuremara’s role as a Registered NDIS Provider, practical steps for participants and families, and how to measure their impact on long-term health outcomes.
Understanding the Health Risks for NDIS Participants
People with disabilities often face complex and interconnected health risks, and the NDIS framework recognises the need for consistent monitoring and support. Many participants experience:
- Difficulty accessing health services
- Communication barriers
- Reliance on others for reporting symptoms
- Co-existing chronic conditions
- Mental health challenges
- Limited mobility or transport access
The NDIS Quality and Safeguards Commission highlights that gaps in regular healthcare access can lead to avoidable emergencies, including severe infections, unmanaged chronic conditions, or complications resulting in extended hospital stays.
Without timely intervention, participants may experience:
- Preventable hospital admissions
- Increased emergency department visits
- Deterioration in functional capacity
- Longer recovery periods
Under the NDIS Practice Standards, providers must support participants’ health and wellbeing by ensuring access to monitoring, early detection, and health assessments.
What Do “Regular Check-Ins” Mean in the NDIS Context?
In the NDIS environment, regular check-ins refer to ongoing touchpoints that ensure participants’ well-being is consistently supported. These include:
Types of Regular Check-Ins
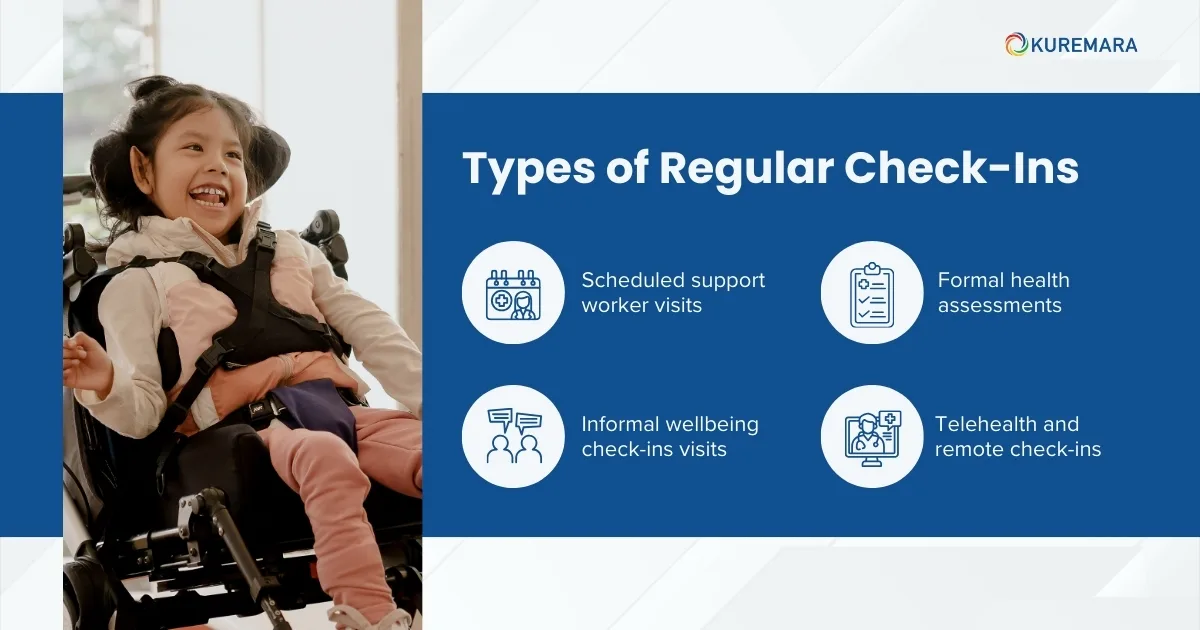
- Scheduled support worker visits: Daily or weekly interactions, tracking physical and emotional changes
- Formal health assessments: Periodic evaluations by allied health or community nursing
- Informal well-being check-ins: Conversations that capture subtle changes in behaviour or mood
- Telehealth and remote check-ins: Virtual contact for participants living remotely or with limited mobility
The NDIS Quality and Safeguards Commission’s Practice Alert on Regular Access to Health Care emphasises consistent monitoring and early intervention.
Regular check-ins can be funded through a range of NDIS support categories, including:
- Daily Living
- Improved Health and Well-being
How Regular Check-Ins Prevent Health Emergencies
1. Early Detection of Health Changes
Regular check-ins help identify signs such as:
- Weight fluctuations
- Reduced mobility
- Changes in appetite
- Fatigue
- Skin concerns
- New behavioural changes
Identifying these signs early often prevents escalation into emergency situations.
2. Stronger Care Coordination
Consistent check-ins enable timely action such as:
- Contacting a GP
- Arranging a nursing assessment
- Mobilising allied health support
- Reviewing medication needs
3. Building Trust and Open Communication
For many participants, particularly those with communication differences, trust is critical. Familiar support workers provide a comfortable environment for participants to raise concerns early.
Example: A participant with chronic respiratory conditions begins showing subtle signs of breathlessness. A weekly check-in by their support worker leads to a prompt GP referral, preventing what could have become a serious hospital for admission.
4. Health and NDIS Plan Benefits
- Reduced emergency admissions
- Smoother support planning
- Enhanced safety
- Higher quality of life
Best Practices for Implementing Regular Check-Ins Under NDIS
For Participants and Families
- Request check-ins as part of your NDIS planning conversation
- Document your health needs clearly in your plan
- Identify which supports require monitoring (medication, nutrition, mobility, mental health)
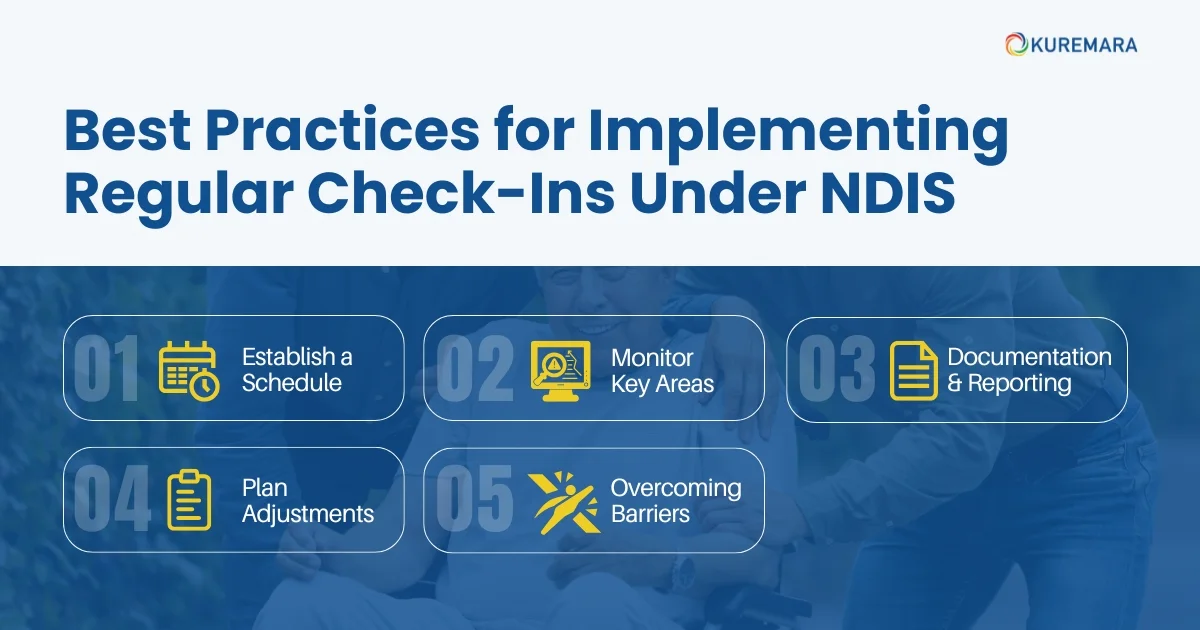
For Support Coordinators and Providers
1. Establish a Schedule
- Decide on a frequency: daily, weekly or monthly
- Tailor visits to each person’s risk profile, age and health conditions
2. Monitor Key Areas
- Basic health indicators (pulse, temperature, fluid intake)
- Medication management
- Mental health and emotional wellbeing
- Functional capacity and mobility
- Communication or behavioural changes
3. Documentation & Reporting
Keep detailed notes on each check-in. These help with:
- Early identification of concerns
- Sharing information with allied health or GPs
- Preparing for NDIS plan reviews
4. Plan Adjustments
Check-ins often reveal evolving needs, which can lead to:
- New support items
- Additional funded hours
- Access to therapy or nursing
- Safeguarding interventions
5. Overcoming Barriers
Participants may face challenges such as:
- Transport limitations
- Communication differences
- Financial concerns
- Rural or remote location
Strategies such as telehealth, accessible communication formats, and culturally safe practice are essential.
How Kuremara Helps Participants and Families Implement Effective Check-Ins
As a Registered NDIS Provider, Kuremara plays a vital role in helping participants and families build a reliable, responsive, and person-centred check-in system.
What Kuremara Does to Keep Participants Safe
1. Routine Wellbeing Visits
Our support workers and community nurses conduct scheduled check-ins tailored to each participant’s needs monitoring daily routines, mood, mobility, hydration, health signs and general wellbeing.
2. Early Identification of Health Risks
Kuremara staff are trained to notice subtle signs that family members may miss, including appetite changes, sleep disturbance, behavioural shifts, or medication concerns. Early detection is key to avoiding emergencies.
3. Coordinated Care and Immediate Response
Whenever our team identifies a potential concern, we:
- Notify families and carers
- Coordinate GP or allied health appointments
- Organise urgent nursing assessments
- Update risk and safety plans
- Communicate with Support Coordinators
This quick action ensures participants receive medical attention before conditions worsen.
4. Accurate Documentation and Reporting
Kuremara records all check-ins, observations and healthcare actions, helping families during:
- Plan reviews
- Requests for additional supports
- Risk management
- Communication with clinicians.
5. Flexible Options: In-Person or Remote
For participants in rural or remote areas or those preferring flexible arrangements, Kuremara offers telehealth-enabled check-ins and digital communication options.
6. Culturally Safe and Inclusive Practices
We ensure that every check-in respects the participant’s culture, preferences, communication style, and comfort.
Role of NDIS Providers and Partners in Check-In Strategy

Registered NDIS providers are responsible for implementing safe, proactive, and evidence-based check-in strategies. Kuremara ensures:
- Consistent monitoring aligned with the NDIS Practice Standards
- Early identification of risks
- Clear communication with families, clinicians and Support Coordinators
- Team-based collaboration with allied health, community nurses and GPs
- Adaptable support for participants with diverse needs
To learn more about accessible and safe support options, visit our blog on Innovations in NDIS Transport.
Measuring Success: What Good Looks Like
Regular check-ins create measurable, positive changes such as:
- Reduced emergency hospital visits
- Increased stability in daily routines
- Better communication between teams
- Improved functional capacity
- Enhanced participant satisfaction
Collecting and Using Data Effectively
Data may come from:
- Provider logs
- GP feedback
- Participant self-reports
- Family observations
This information helps refine NDIS plans, improve safety plans and strengthen long-term support strategies.
Conclusion
Regular check-ins are one of the most effective ways to prevent health emergencies for NDIS participants. When implemented consistently, they help identify health changes early, strengthen care coordination, and provide a safety net that supports ongoing independence and wellbeing.
At Kuremara, we ensure that every visit truly counts. Our team works closely with participants and their families to integrate meaningful check-ins into daily routines and NDIS plans, ensuring proactive, compassionate and reliable support.
If you or your loved one need a trusted provider that prioritises safety, wellbeing and early intervention, Kuremara is here to help.
FAQs
1. What frequency of check-in is recommended?
A. It depends on the participant’s needs, health conditions, and risks. Some may require daily visits, while others may benefit from weekly or monthly check-ins.
2. Are check-ins funded under the NDIS?
A. Yes. They may fall under Daily Living, Support Coordination, Community Nursing or Capacity Building supports.
3. What happens if a check-in uncovers a serious issue?
A. Kuremara coordinates immediate action, contacting GPs, arranging nursing assessments or requesting urgent plan reviews if required.
4. Can check-ins be done remotely?
A. Yes. Telehealth or virtual check-ins help support participants in rural or remote areas or those who prefer digital communication.
5. Who documents the check-ins?
A. Support workers, nurses and providers like Kuremara record check-in details and share relevant information with families and clinicians.
 care@kuremara.com.au
care@kuremara.com.au