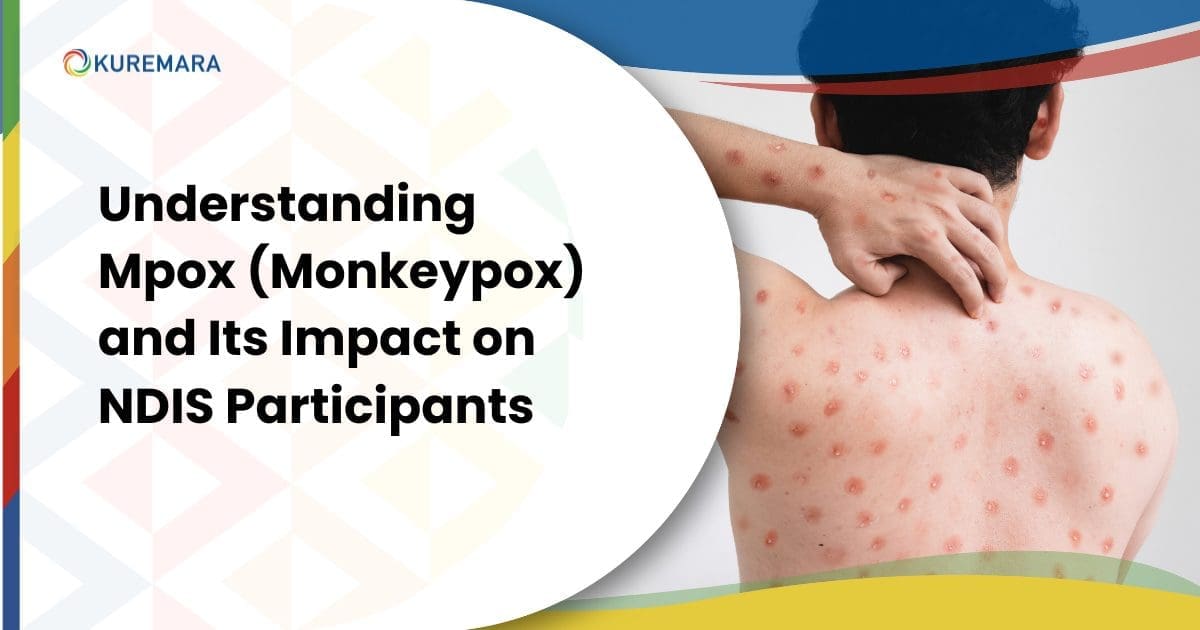
Mpox, previously known as monkeypox, is a viral disease that has raised global health concerns due to its rapid spread and the potential risks it poses, particularly for vulnerable communities like NDIS participants. As the World Health Organisation (WHO) has declared Mpox a public health emergency of international concern, it’s essential for NDIS participants and providers to stay informed about the disease, its symptoms, preventive measures, and how it can be managed within the NDIS framework.
What is Mpox?
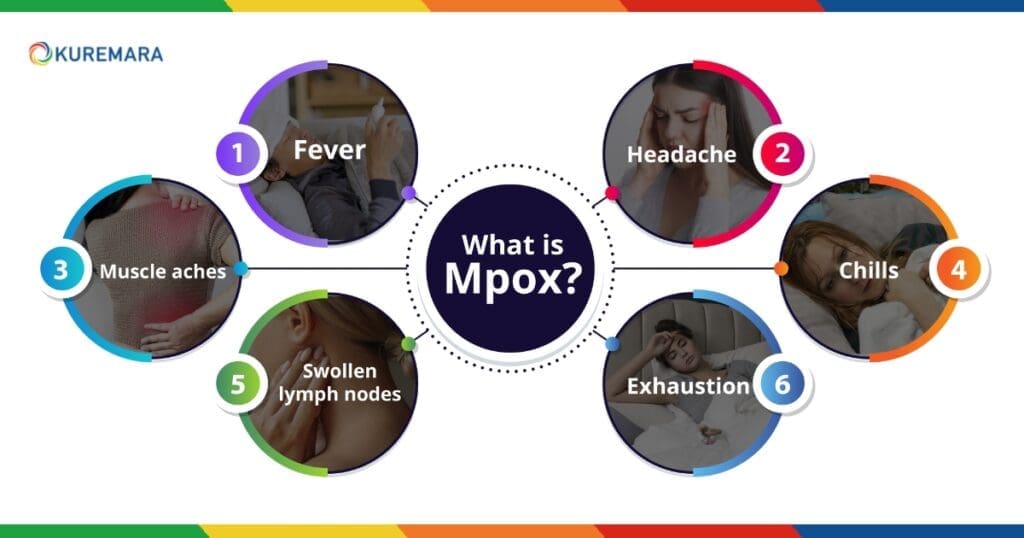 Mpox is a zoonotic viral disease, meaning it can spread from animals to humans, although human-to-human transmission is also common. The virus belongs to the same family as the smallpox virus but is generally milder. Symptoms typically appear within 5 to 21 days after exposure and can last between 2 to 4 weeks. Common symptoms include:
Mpox is a zoonotic viral disease, meaning it can spread from animals to humans, although human-to-human transmission is also common. The virus belongs to the same family as the smallpox virus but is generally milder. Symptoms typically appear within 5 to 21 days after exposure and can last between 2 to 4 weeks. Common symptoms include:
- Fever
- Headache
- Muscle aches
- Swollen lymph nodes
- Chills
- Exhaustion
- A distinctive rash that often starts on the face and spreads to other parts of the body, including the hands, feet, and genitals.
Mpox primarily spreads through direct contact with bodily fluids, skin lesions, or contaminated objects like bedding or clothing. Prolonged face-to-face contact can also lead to transmission via respiratory droplets.
Why is Mpox a Concern for NDIS Participants?
 For NDIS participants, particularly those with disabilities or chronic health conditions, the risks associated with Mpox are heightened. Many participants rely on close personal care, which can increase the risk of exposure to infectious diseases like Mpox. Additionally, those with mobility challenges or cognitive impairments may struggle to adhere to strict hygiene and preventive practices, making them more vulnerable.
For NDIS participants, particularly those with disabilities or chronic health conditions, the risks associated with Mpox are heightened. Many participants rely on close personal care, which can increase the risk of exposure to infectious diseases like Mpox. Additionally, those with mobility challenges or cognitive impairments may struggle to adhere to strict hygiene and preventive practices, making them more vulnerable.
The impact of Mpox on NDIS participants can be severe, especially if they have compromised immune systems. In some cases, the infection could lead to serious complications, emphasising the need for proactive measures to protect this vulnerable group.
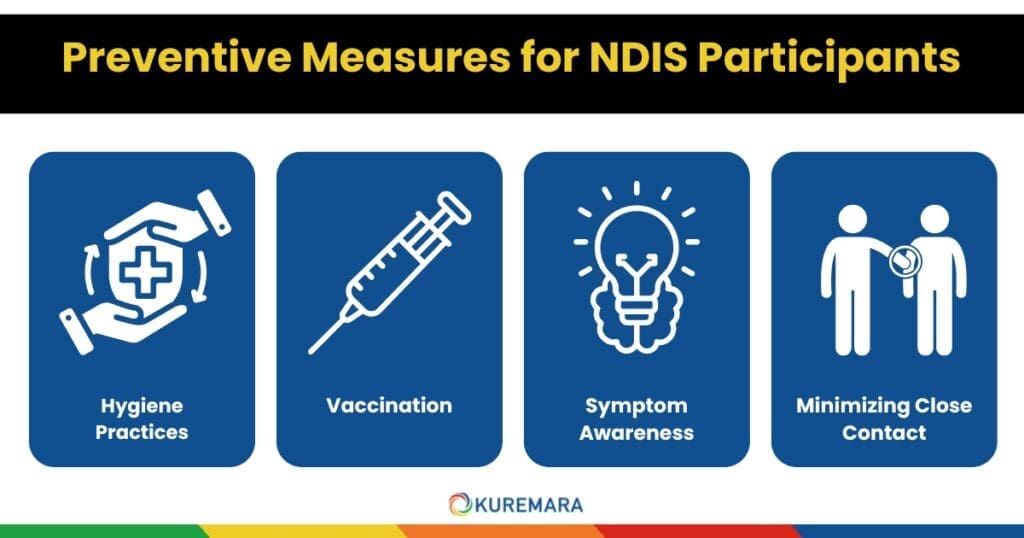
Preventive Measures for NDIS Participants
Preventing the spread of Mpox among NDIS participants is crucial. Here are some key steps:
Hygiene Practices
Regular handwashing with soap and water, as well as using hand sanitisers, is vital. NDIS support workers should be trained in hygiene protocols to minimise the risk of virus transmission.
Vaccination
If vaccines are available and recommended by health authorities, they can be an effective preventive measure. NDIS participants and their carers should stay informed about the availability of vaccines and consult healthcare providers on whether vaccination is appropriate.
Symptom Awareness
Participants and carers should be educated about Mpox symptoms and encouraged to seek prompt medical help if they notice any signs. Early detection and isolation are crucial in preventing the spread of the virus.
Minimising Close Contact
During an outbreak, reducing close physical interactions is essential. Remote support services and alternative care strategies can help maintain essential support while minimising the risk of transmission.
The Role of NDIS Providers in Managing Mpox
NDIS providers like Kuremara play a critical role in ensuring the safety and well-being of participants during public health crises like the Mpox outbreak. Here’s how Kuremara and other NDIS providers can manage the situation:
Staff Training and Awareness
Ensure all care workers are well-informed about Mpox symptoms, transmission methods, and preventive measures. Regular updates should be provided based on the latest public health guidelines.
Implementing Safety Protocols
Introduce strict hygiene practices, regular health checks, and screening for both participants and staff. Proper use of personal protective equipment (PPE) should be enforced when providing care.
Adapting Services
Providers should offer telehealth consultations and other remote services to reduce the need for in-person interactions. This is especially important for high-risk participants who require continuous care but are vulnerable to infection.
Communication and Support
Keep participants and their families informed about the ongoing risks and safety measures. Open and transparent communication helps build trust and ensures everyone is aware of what steps are being taken.
Accessing Health Services Through NDIS
 If an NDIS participant shows symptoms of Mpox, it is important to act quickly. Here are some steps to take:
If an NDIS participant shows symptoms of Mpox, it is important to act quickly. Here are some steps to take:
Contact a Healthcare Provider
Participants should reach out to their GP or a healthcare professional immediately. Telehealth services can provide a safer alternative to in-person visits.
Inform the NDIS Support Coordinator
Notify the participant’s support coordinator so that any additional care or resources needed can be arranged promptly.
Use NDIS Funding for Health Services
NDIS funding can be utilised for accessing necessary health services, including consultations, medications, and specialised care.
Follow Public Health Guidelines
Adherence to public health advice, including isolation when recommended, is key to preventing the virus from spreading.
What is the Australian Government Doing?
Australia’s response to Mpox focuses on monitoring, public education, and vaccination. The Department of Health provides updated information and guidance, while NSW Health continues to release updates to keep the public informed. Public health campaigns aim to raise awareness and equip communities with the tools needed to protect themselves.
Conclusion
The emergence of diseases like Mpox highlights the importance of preparedness and awareness, especially for vulnerable communities like NDIS participants. By staying informed, practicing good hygiene, and following recommended public health guidelines, both participants and providers can navigate health crises more effectively.
At Kuremara, we are committed to ensuring our participants receive the essential support and guidance they need during such challenging times. For more information on how Kuremara can assist you, please visit our website or contact our support team.
For the latest updates on Mpox, visit the Australian Department of Health and WHO.
 care@kuremara.com.au
care@kuremara.com.au



Write a comment
Your email address will not be published. All fields are required