Imagine a child in the classroom, struggling to suppress sudden, repetitive movements or sounds. Their classmates may not understand, and even teachers might mistake their actions for misbehavior. This is the reality for many individuals with Tourette Syndrome (TS), a condition that is often misunderstood and stigmatised.
Tourette Syndrome is a neurological disorder characterised by involuntary tics—sudden, repetitive movements or vocalisations. While some individuals experience mild symptoms, others face significant challenges in daily life, including difficulty with social interactions, barriers to education, and emotional distress due to stigma and misunderstanding.
This blog aims to provide a comprehensive understanding of Tourette Syndrome, dispel common myths, and explore its eligibility for National Disability Insurance Scheme (NDIS) funding. For individuals living with TS and their families, accessing the right support can make a world of difference.
Introduction to NDIS
The NDIS (National Disability Insurance Scheme) is an Australian government initiative designed to provide financial and practical support to individuals with disabilities. It aims to improve their quality of life by funding services such as therapy, assistive technology, and daily support. But does Tourette Syndrome qualify for NDIS support? Let’s find out.
What is Tourette Syndrome?
Tourette Syndrome is a neurological condition that causes individuals to experience repetitive, involuntary movements and vocalisations known as tics. It is a lifelong disorder, but symptoms often fluctuate over time and can improve with age.
Core Symptoms
- Tics: These are sudden, brief, and repetitive movements or sounds.
- Simple vs. Complex Tics: Simple tics include behaviors like eye blinking, throat clearing, or shoulder shrugging. Complex tics involve coordinated patterns of movement or the utterance of words and phrases.
- Fluctuating Nature: The severity of tics can change over time, sometimes worsening during periods of stress or excitement and diminishing during periods of relaxation.
Associated Conditions
Many individuals with TS also experience co-occurring conditions that can impact their daily functioning, such as:
- Attention Deficit Hyperactivity Disorder (ADHD): Difficulty with attention, impulsivity, and hyperactivity.
- Obsessive-Compulsive Disorder (OCD): Persistent, unwanted thoughts and repetitive behaviors.
- Anxiety Disorders: High levels of stress and worry, which can exacerbate tics.
- Learning Difficulties and Behavioral Challenges: Some individuals with TS may struggle with executive function, emotional regulation, or sensory sensitivities.
Causes and Risk Factors
While the exact cause of Tourette Syndrome is unknown, research suggests a combination of genetic and environmental factors contributes to its development. It often runs in families, indicating a strong hereditary component.
Tourette Syndrome: Myths and Facts
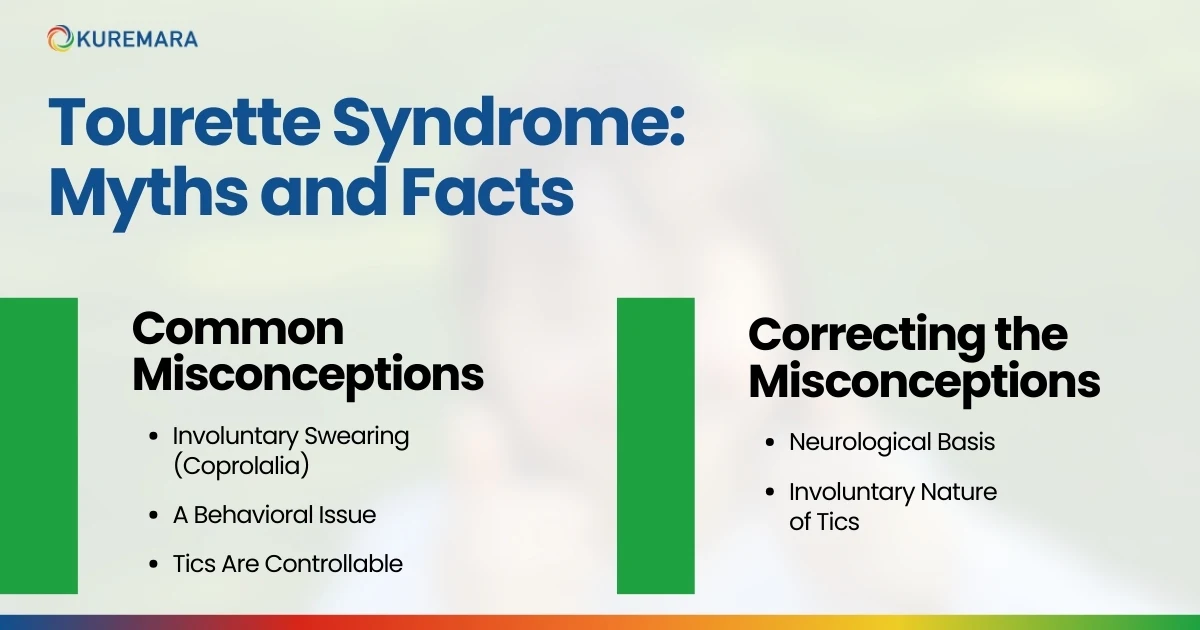
Common Misconceptions
- Involuntary Swearing (Coprolalia): A widely held myth is that all individuals with TS engage in involuntary swearing. In reality, only about 10-15% of those with TS exhibit coprolalia.
- A Behavioral Issue: Many people mistakenly believe that Tourette Syndrome is a behavioral disorder, rather than a neurological condition.
- Tics Are Controllable: While some individuals may temporarily suppress their tics, doing so is often uncomfortable and exhausting.
Correcting the Misconceptions
- Neurological Basis: TS is caused by differences in brain function and structure, particularly in the basal ganglia and neurotransmitter systems.
- Involuntary Nature of Tics: Tics are not performed deliberately; they occur as a result of neural activity beyond the individual’s control.
Diagnosis and Management
1. Diagnostic Criteria
Tourette Syndrome is typically diagnosed based on the following criteria:
-
- Presence of multiple motor tics and at least one vocal tic.
-
- Symptoms persisting for more than one year.
-
- Onset before the age of 18.
-
- No other medical condition explaining the symptoms. Diagnosis should be confirmed by a medical professional, such as a neurologist or psychiatrist, based on clinical evaluation and patient history.
2. Treatment Options
-
- Comprehensive Behavioral Intervention for Tics (CBIT): A therapy that teaches individuals strategies to manage and reduce tics.
-
- Medications: In severe cases, medications such as antipsychotics or alpha agonists may be prescribed.
-
- Lifestyle Adjustments: Strategies like stress management, physical exercise, and a structured routine can help manage symptoms.
3. Is There a Cure?
There is currently no cure for Tourette Syndrome, but many people experience a significant reduction in tics over time. Proper treatment can help individuals manage their symptoms and improve their quality of life.
4. Prevention
Because Tourette Syndrome has a strong genetic component, there is no known way to prevent it.
Who is Most Affected?
-
- TS typically emerges in childhood, between the ages of 5 and 10.
-
- Males are three to four times more likely to be diagnosed with TS than females.
Impact Across the Lifespan
While many individuals experience a reduction in tics during adolescence or adulthood, some continue to face challenges that require ongoing support.
Tourette Syndrome and NDIS Eligibility
1. Does Tourette Syndrome Qualify?
Eligibility for NDIS is based on the extent to which a condition impacts daily functioning. Individuals with severe TS who experience difficulties with communication, learning, self-care, or mobility may qualify.
2. How to Apply for NDIS with Tourette Syndrome
- Gather Evidence: Obtain reports from neurologists, psychologists, or occupational therapists.
- Supporting Documentation: Include information about how tics impact daily life and participation in activities.
NDIS Support for Tourette Syndrome
1. Types of Support Available
-
- Therapy (CBIT, speech therapy, occupational therapy).
-
- Support coordination.
-
- Social skills training.
2. What a Registered NDIS Provider Can Offer
NDIS providers, like Kuremara, can assist with therapy, daily living support, and access to specialists who understand TS.
Creating the Perfect NDIS Plan for Tourette Syndrome

- Identifying Goals and Needs – A well-structured plan should reflect individual challenges and aspirations.
- Working with Support Coordinators – Support coordinators assist in managing the plan and ensuring participants receive appropriate services.
- Regular Plan Reviews – Reviewing and updating the plan helps individuals adapt to changing needs.
Conclusion
Raising awareness about Tourette Syndrome is crucial in breaking down misconceptions, reducing stigma, and ensuring that individuals with TS receive the support they need to lead fulfilling lives. Education and advocacy play a significant role in fostering a more inclusive society.
 care@kuremara.com.au
care@kuremara.com.au